CPR stands for cardiopulmonary resuscitation – or in plain English, artificially (and partially) restoring the function of the heart and lungs of an unconscious, pulseless person. As blood flow (perfusion) is critical in the survival of major organs such as the brain, this procedure can save lives by prolonging a victim’s life until the paramedics arrive to provide professional medical care.
When the heart stops beating, or becomes inefficient due to erratic beating, blood flow stops. In the case of the brain, this means that the cells will start dying after 4~5 minutes if perfusion is not restored. CPR can restore about 30% of perfusion, delaying the onset of brain death.
This may be critical when someone suffers a heart attack (myocardial infarction) and paramedics will not arrive for over 10 minutes. Ergo, this is one of the most important emergency skills one should know to help people in need as soon as possible.
There are different guidelines for CPR in many countries, but here is a standard procedure guideline (NZ).
It is summarised into the acronym: DR’S ABCD (doctor’s ABCD), and is a flowchart that goes from one step to the next (detailed explanation after summary).
- Danger: check that area is safe and risk-free
- Response: check for patient response by shouting, shaking, pain
- Send for help: pick one person to call emergency services
- Airway: check airway, remove obstruction, tilt head back and lift chin
- Breathing: check for breathing, go to CPR if no breathing
- Circulation: check for pulse if breathing, if no pulse, start CPR (30 chest compressions : 2 breaths)
- (Defibrillation): follow AED instructions

The first rule of first aid is that you must not put yourself in danger. For example, if the patient is on the road, pull them to a safe area to minimise the risk to your own health.
Then, check for a response. The easiest way is to call loudly to them such as “Can you hear me”, and inflicting pain (such as rapping on their chest or shaking their shoulders) and see if they become conscious.
If they remain unconscious, immediately designate a person around you by pointing to them (otherwise they will be less likely to be responsible) to call the emergency service (111, 911, 119 etc.), alerting them the location and state of the patient.
This is the point when clinical skills come in.
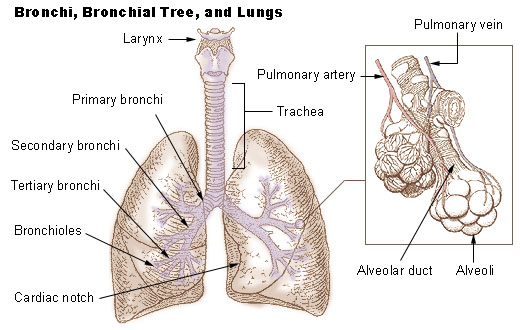
Airway: An unconscious person may have their airway obstructed by vomit or their own tongue (which falls back by gravity into the throat). You must secure the airway by scooping out any material, and clearing the tongue out of the way. This is done by tilting the head back far (as if they are looking up), then using one hand to pull their chin out. This opens the airway up so that mouth-to-mouth becomes effective.
Breathing: Put one ear right next to the person’s nose and mouth and check for any breathing sounds or air flow. If they are breathing, check the pulse to see if they are pumping blood. If not, go straight to CPR.
Circulation: It is best to check the central pulses such as the carotid (side of neck, next to the Adam’s apple), brachial (squeeze inner side of biceps) or femoral pulses. The carotid is often the easiest as most people know how to take it. If you feel a pulse, put the patient in recovery position as they are just unconscious, breathing and has blood flowing. If not, proceed to CPR (as you do with when the patient is not breathing).
CPR is composed of two actions: chest compressions and mouth-to-mouth breathing. The former is the strong compression of the chest wall to squeeze blood in and out of the heart; the latter is breathing air into the patient’s lungs and letting exhalation come out naturally.
Chest compressions are often misrepresented in medical dramas, and is extremely important that you do it correctly. First find where the sternum is (centre of ribcage, between the nipples) and place the heel of your left palm on it, then spread your fingers out. Put your right hand over your left and close your fingers around it for a good grip. If the patient is lying flat on the ground (with head tilted back), kneel beside them and stoop over their chest with straight, locked arms (bent arms exert much less pressure).
You are now ready to begin chest compressions. Press down hard, until the chest wall is compressed to about 1/3~½ depth (the chest wall is a springy structure, and do not worry about broken ribs, as being alive is more important for the person), then ease pressure to let it bounce back up. Ideally the time pushing and the time letting it bounce back should be the same, giving a good rhythm. Repeat this 30 times at the beat of 100/min, or in easier terms: to the beats of the Bee Gee’s song Stayin’ Alive (scientifically proven).
After 30 compressions, tilt the patient’s head back, lift their chin up, and lock your mouth over their mouth and nose to make an airtight seal. It is crucial that you use a face shield to prevent the spread of disease. Be aware that breaths are less important than the compressions, so if you do not have a face shield, let someone else do the breathing and focus on chest compressions. Pinch the nose closed to ensure air does not escape.
Forcefully breathe into them and look for the chest rising. Let go of the nose and pull away so that they can breathe out. Repeat once, then return to chest compressions.
After 2 minutes of CPR (30 compressions : 2 breaths, repeat 4 times), change places with another person capable of CPR, as otherwise you will tire out and become inefficient.
Defibrillation is only possible if you are near an AED (automated external defibrillator). Nowadays, AEDs are designed to be completely user-friendly so simply follow the instructions on the machine.
It is important to note that not all abnormal heart rhythms are “shockable” (see Flatline). Follow the AED’s instruction, as it will state whether shock is advised or not. Make sure that CPR is still happening continuously.
Repeat until help arrives.
As a final note, remember that the patient is dead whether you do CPR or not, so there is nothing to lose. Believe it or not, this will be of incredible help in calming your mind when struck with such an emergency. Even with CPR, there is a maximum 30% chance the patient will survive, 10% if it occurs outside the hospital. But if you do nothing, their survival chance will be 0%, so put all your energy into resuscitating them, and you may just save a life.